Complete Guide to PBS Costs and Coverage in Australia
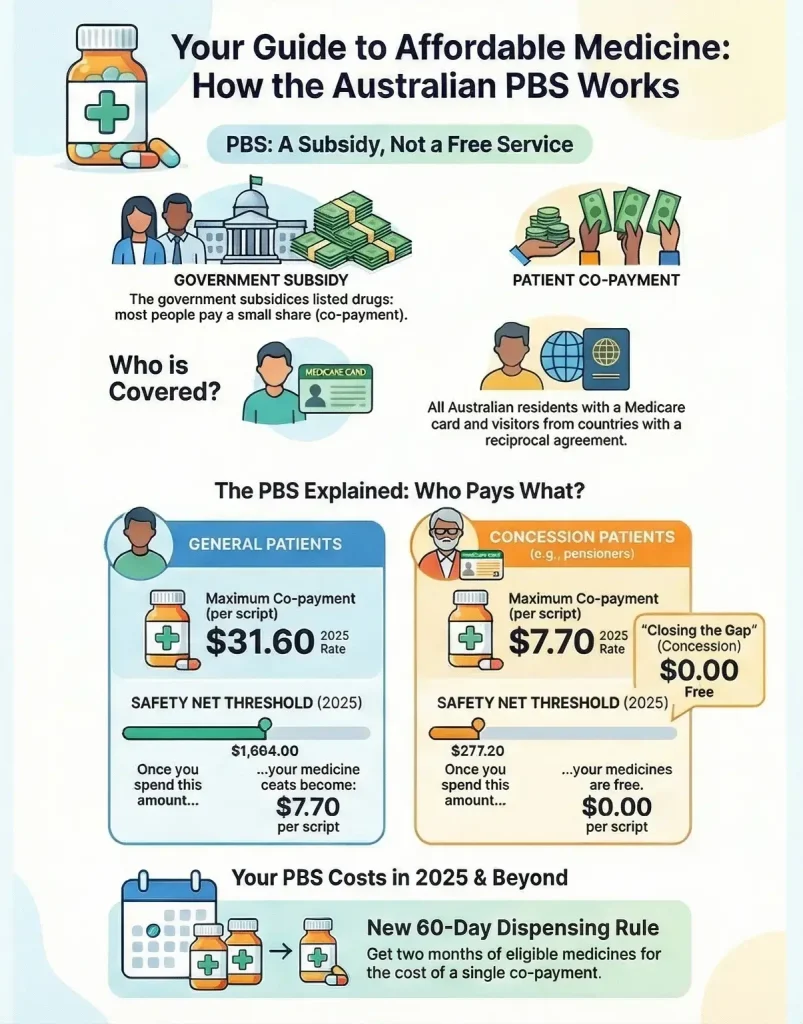
The Pharmaceutical Benefits Scheme (PBS) is a cornerstone of Australia’s public health system, designed to provide reliable, timely, and affordable access to a wide range of necessary medicines. Managed by the Department of Health and Aged Care and administered by Services Australia, the PBS ensures that no Australian is denied access to essential medication due to cost. This guide breaks down how the scheme works, who is eligible, and the costs involved for the 2025 calendar year.
What the PBS Is and Why It Exists
The PBS is a government-funded subsidy program that lowers the cost of prescription medicines for consumers. Without this scheme, the cost of many life-saving drugs—such as those for cancer, diabetes, or heart disease—would be prohibitively expensive for the average person, often costing thousands of dollars per script.
The primary purpose of the PBS is to keep essential medicines affordable. The Australian Government subsidises the cost of listed medicines, meaning patients pay only a small portion of the actual price (a “co-payment”), while the government covers the rest. This system balances the need for a sustainable healthcare budget with the goal of equitable health outcomes for all residents.
Who Can Access PBS Medicines
Access to the PBS is broad but specific to certain groups:
- Australian Residents: Anyone who holds a valid Medicare card is eligible for PBS-subsidised medicines.
- Concession Card Holders: Pensioners, veterans (DVA card holders), and holders of Health Care Cards or Commonwealth Seniors Health Cards are eligible for further reduced rates.
- Reciprocal Health Care Agreements (RHCA): Visitors from countries with a reciprocal agreement with Australia (including the UK, Ireland, New Zealand, Malta, Italy, Sweden, the Netherlands, Finland, Norway, Belgium, and Slovenia) can access the PBS. They must show their passport or a reciprocal health care card.
How the PBS Works
The scheme operates on a co-payment model. When a doctor prescribes a PBS-listed medicine, the patient does not pay the full market price. Instead, they pay a capped contribution known as a “co-payment.”
- Patient Co-payment: This is the maximum amount a patient pays for a standard PBS medicine.
- Government Contribution: The government pays the pharmacy the difference between the patient’s co-payment and the agreed price of the drug.
- General vs. Concession: The system is two-tiered. “General” patients (most working adults) pay a higher co-payment, while “Concession” patients (pensioners and low-income earners) pay a significantly lower rate to ensure affordability.
What Medicines Are Covered
The list of medicines subsidised by the government is known as the PBS Schedule.
- Selection Process: Medicines are not added automatically. They must be assessed by the Pharmaceutical Benefits Advisory Committee (PBAC), an independent expert body of doctors, health professionals, and economists. The PBAC recommends medicines based on their clinical effectiveness, safety, and cost-effectiveness (value for money) compared to existing treatments.
- PBS vs. Non-PBS: Not every medicine is on the PBS. Some drugs are “private,” meaning the manufacturer’s price was not accepted by the government, or the condition treated does not meet the strict funding criteria. In these cases, patients must pay the full price.
Understanding PBS Costs (2025 Rates)
For the 2025 calendar year, the costs are structured as follows. Note that co-payment amounts have been subject to a freeze to help with cost-of-living pressures.
- General Co-payment: Up to $31.60 per script.
- Concessional Co-payment: Up to $7.70 per script.
- Closing the Gap (CTG): Registered Aboriginal and Torres Strait Islander people pay a reduced co-payment. General patients under CTG pay the concession rate ($7.70), while concession card holders under CTG receive medicines for free.
- Discretionary Discount: Pharmacists may offer a small discount (up to $1.00) on the co-payment, though due to indexation rules in 2025, the effective discount is often capped lower (e.g., $0.10 for general patients).
| Category | Patient Cost | Notes |
|---|---|---|
| General Co payment | Up to 31.60 per script | Standard rate for general patients |
| Concessional Co payment | Up to 7.70 per script | Applies to eligible concession card holders |
| Closing the Gap CTG | General patients pay 7.70. Concession patients pay zero | Available to registered Aboriginal and Torres Strait Islander people |
| Discretionary Discount | Up to 1.00 discount. Often lower in 2025 due to indexation for example 0.10 for general patients | Applied at pharmacist discretion |
Brand and Group Premiums
Sometimes, you may pay more than the standard co-payment. This happens if you choose a more expensive brand when a cheaper, equally effective one exists.
- Brand Premium: An extra cost for a specific brand name (e.g., the originator brand) when a cheaper generic version is available. The government only subsidises the price of the cheaper version.
- Therapeutic Group Premium: Applies when you choose a medicine in a group (e.g., blood pressure tablets) that is more expensive than a similar medicine in the same therapeutic class.
- Note: These premiums do not count toward your Safety Net threshold.
The PBS Safety Net Explained
The PBS Safety Net protects patients and families requiring a high volume of medicines. Once your total spend on PBS co-payments reaches a certain threshold in a calendar year, medicines become cheaper or free for the rest of that year.
- 2025 General Safety Net Threshold:$1,694.00.
- Benefit: Once reached, general patients pay the concession rate ($7.70) for the remainder of the year.
- 2025 Concession Safety Net Threshold:$277.20.
- Benefit: Once reached, concession patients receive PBS medicines for free for the remainder of the year.
Prescription Requirements
To access the subsidy, the prescription must be written correctly:
- Regular Prescriptions: Standard scripts for most medicines.
- Authority Prescriptions: Required for certain expensive or dangerous drugs. The doctor must obtain approval (or use a specific “streamlined” code) to confirm the patient meets the specific clinical criteria (indications) for funding.
- Restricted Benefits: Some medicines are only subsidised for specific conditions (e.g., a drug might be PBS-listed for severe severe asthma but not for a mild cough). If used for a non-listed condition, it is a private script.
Private Prescriptions vs PBS Prescriptions
A “Private Prescription” means the government provides no subsidy. This occurs when:
- The medicine is not listed on the PBS.
- The patient’s condition does not meet the clinical criteria (indications) for the subsidy.
- The medicine costs less than the co-payment amount (meaning the patient pays the full price anyway, though this often still counts toward the Safety Net if recorded).
Cost Differences: Private scripts can be significantly more expensive. Private health insurance (extras cover) may sometimes rebate a portion of non-PBS prescriptions, but this varies by policy.
How to Check if a Medicine Is on the PBS
Patients can easily verify the status of a medicine:
- PBS Website: Visit pbs.gov.au and type the medicine name in the search bar.
- Item Codes: Look for the specific “Item Codes” which denote the strength and form (e.g., tablet, injection) covered.
- Listings: The site details the “Max Qty” (maximum quantity per pack) and “Repeats” (number of times you can refill it), as well as any “Authority Required” restrictions.
Common Myths About the PBS
- “The PBS is free.”
- Fact: It is a subsidy, not a free service (unless you are a concession holder who has reached the Safety Net). Most people pay a co-payment.
- “Every medicine approved for use in Australia is on the PBS.”
- Fact: The TGA (Therapeutic Goods Administration) approves medicines for safety, but the PBS only lists them if they are cost-effective. Many safe medicines are available only on private prescription.
- “PBS and Medicare are the same thing.”
- Fact: They are separate schemes. Medicare subsidises medical services (doctors, hospitals), while the PBS subsidises medicines.
Recent Updates and Policy Changes (2024-2025)
- 60-Day Dispensing: A major reform fully rolled out by late 2024. Patients with stable chronic conditions can now receive 60 days’ supply of eligible medicines (approx. 300 items) for the cost of a single co-payment. This effectively halves the cost of medicines for these patients.
- Co-payment Freeze: To assist with cost of living, the general co-payment of $31.60 has been frozen for 2025, and the concession co-payment of $7.70 has been frozen for five years (until 2029).
- Closing the Gap Expansion: From January 1, 2025, the “Closing the Gap” PBS Co-payment program was expanded to cover PBS medicines dispensed in public hospitals, further improving access for First Nations people.
Final Thoughts
The Pharmaceutical Benefits Scheme is a vital asset to the Australian health system, protecting citizens from the high cost of modern pharmaceuticals. By understanding how the Safety Net, co-payments, and generic brands work, patients can make informed choices to manage their health expenses effectively. Whether you are a general patient or a concession card holder, the PBS ensures that financial status is not a barrier to receiving necessary medical treatment.
Article Sources